International trial of blood thinners for COVID-19 treatment begins
by Dr. Liji Thomas, MDA recent news release by the National Institutes of Health (NIH) announces the start of two Phase 3 clinical trials to explore blood thinners as treatments for COVID-19.
These trials, known as ACTIV-4 Antithrombotics, are part of the three planned adaptive trials in this area of clinical research, included in the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) initiative. They are expected to yield new data on the safety and efficacy of these drugs in the treatment of active and convalescent COVID-19 treatment.
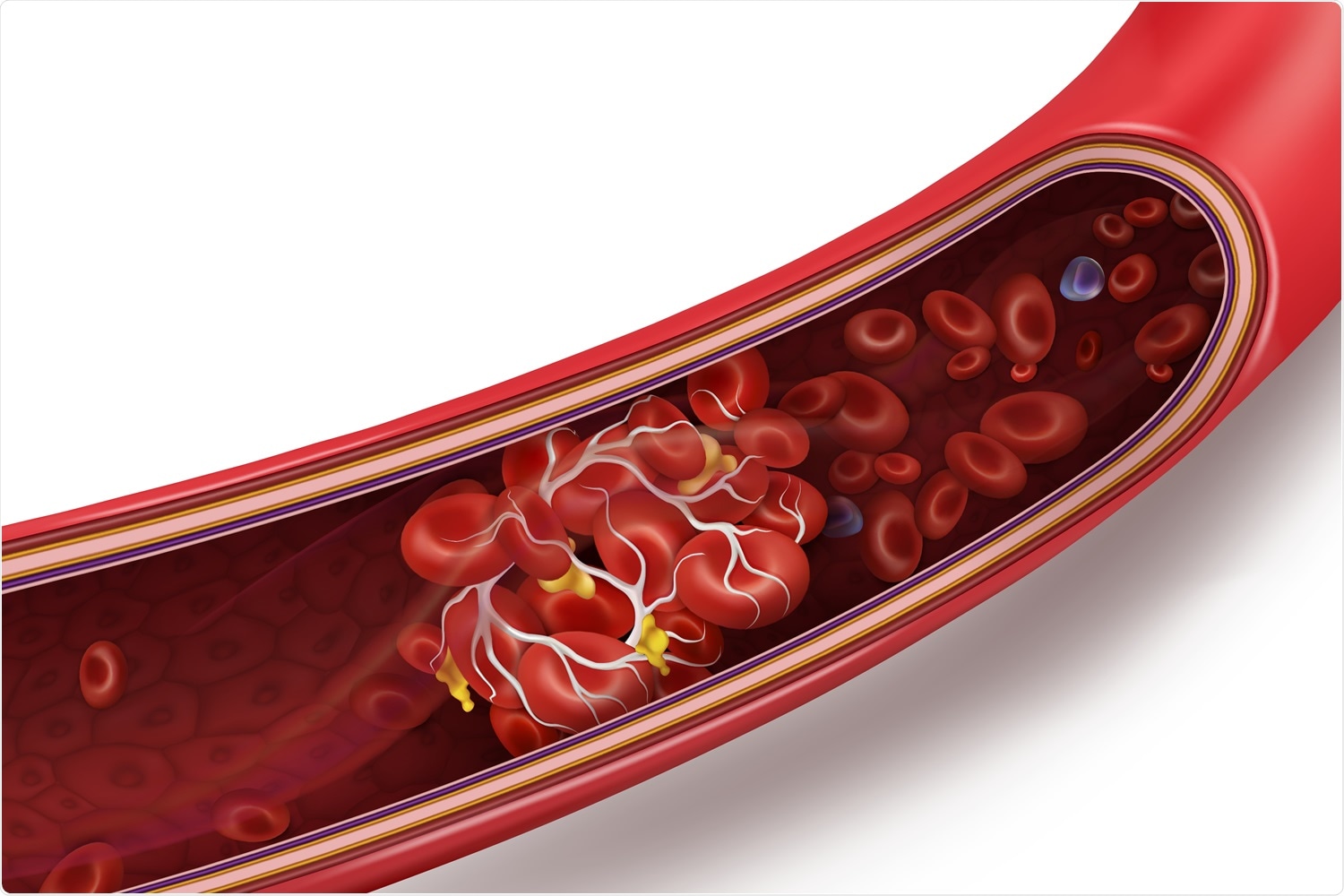
Image Credit: Studiovin / Shutterstock
The Trial Rationale
Many studies have demonstrated the presence of multiple clots in medium and microscopic vasculature. This is a dreaded complication since it may be associated with organ damage, cerebrovascular attacks, heart attacks, and pulmonary embolism.
The results from these trials will be important to understand if and how anticoagulant therapy can help patients with COVID-19. They are funded by Operation Warp Speed, the presidential initiative to speed up the development of effective therapeutics for this condition.
Trial Design
These trials will incorporate data from over a hundred centers the world over, involving patients in various phases of the disease (not hospitalized, currently hospitalized, and discharged from hospital after recovering from moderate to severe disease). The currently starting trials include those in the first two categories.
The ACTIV-4 Antithrombotics trial centers are being carried out at places where there is a high prevalence of COVID-19, in order to recruit patients for treatment with different blood thinners. The study has an adaptive design – the number, type, and dosage regimes of the various anticoagulants can be varied throughout the trial period in accordance with emerging data, so as to minimize the time required to arrive at definite results for these drugs without unacceptable safety issues.
The Currently Hospitalized Patient arm of the trial, called the ACTIV-4 Antithrombotics Inpatient Arm, will look at how different doses of heparin affect clotting risk and outcomes in hospitalized patients. Low and high doses have been determined, with the addition of other drugs as evidence comes in during the trial. Standard care will continue for all patients as required on an individual basis.
The ACTIV-4-Antithrombotics Outpatient arm is to test the role of anticoagulants on potentially lethal cardiovascular and lung complications in patients with mild disease. In addition, their demographic, clinical, and laboratory data, as well as blood samples, will be retrieved to help pick out useful new targets for treatment and biomarkers that can predict the risk of complications in this condition. This arm will be placebo-controlled, with three intervention groups receiving aspirin, low-dose, and high-dose apixaban, respectively.
The Trial Objectives
The role of these drugs is to keep blood proteins and platelets from clumping and forming clots. The challenge facing researchers in COVID-19 is to find out the point at which this intervention will be effective. Says NIH Director Francis Collins, “There is currently no standard of care for anticoagulation in hospitalized COVID-19 patients, and there is a desperate need for clinical evidence to guide practice.”
The investigators aim at finding ways in which to enhance the natural anticoagulation activity of the blood to reduce these complications in COVID-19. Heparin is showing the potential to fulfill this role, but clinical data will be needed to find out the right dose and what other medications should be added. Many universities are involved in the planning of the trial and development of protocols and analytics.
This is a public-private partnership aimed at developing a coordinated response to facilitate the development of new therapies and vaccines for this condition. A later third study is planned to test for the effect of blood thinners on recovered patients with negative RT PCR tests to explore the chances of reducing the risk of blood clots in convalescence.
Advantages
The design of these trials, where existing networks are pieced together to obtain large-scale simultaneous rapid testing of anticoagulants, will help bring quicker results.
As Gary Gibbons, Director of NHLBI, says, “Harnessing and integrating the assets within existing networks gives us an enormous head start and will allow us to get answers much sooner.” The researchers are hopeful that the design will enable the study to be completed in months, and not years, giving them “a clear sense what is the most beneficial way” of integrating anticoagulants into the treatment process.
Sources:
- Nih.gov. (2020). NIH ACTIV Initiative Launches Adaptive Clinical Trials of Blood-Clotting Treatments For COVID-19. https://www.nih.gov/news-events/news-releases/nih-activ-initiative-launches-adaptive-clinical-trials-blood-clotting-treatments-covid-19. Accessed September 12, 2020.
- Moreno, J. E. et al. (2020). Researchers Begin Clinical Trials Examining Blood Thinners as Coronavirus Treatment. https://thehill.com/policy/healthcare/515935-researchers-begin-clinical-trials-examining-blood-thinners-as-coronavirus. Accessed on 09/10/20.