
Tired staff, but pushing on: How TTSH-NCID responded to COVID-19 from day one
by Christy Yip,CNA Insider trailed staff from Tan Tock Seng Hospital and the National Centre for Infectious Diseases through the lulls, surges and uncertainty of the pandemic. After eight months, their jobs are not any easier. Are they prepared for the next wave?
SINGAPORE: The team from Tan Tock Seng Hospital (TTSH) and the National Centre for Infectious Diseases (NCID) has been here before.
For the first time since February, there are only around 20 COVID-19 patients warded in the NCID. At its peak, it had around 500 patients.
The NCID screening centre, led by TTSH’s emergency department, is scaling down. And it feels almost like it was when CNA Insider first met the team.
During the lull of late February to early March, Singapore’s recovery rates outpaced infections. And going back to business as usual was an option for the hospital.
But it soon proved to be the last thing possible when travellers and returning Singaporeans brought a wave of cases to the screening centre. For close to seven months, our cameras kept rolling.
In our final interview with Charmaine Manauis, who is part of the team leading efforts at the screening centre, the doctor finally does not look like she is rushing somewhere.
We ask her how she feels looking back, now that things have quietened down. While she is usually composed, words fail her at this point.
She thinks of the manpower that came together to run the screening centre, and begins to tear up. “The screening centre is going to (be here for) a long time,” she says.

We remember, once again, the weight of a hospital’s work in this crisis and how drawer plans were put to the test, pivots were made and lessons learned.
This is an exclusive look behind the scenes at Singapore’s dedicated outbreak facility and how TTSH-NCID fought the COVID-19 battle to come out on top so far.
THE SCREENING CENTRE ENTERS THE STORM
On the afternoon of Mar 24, we receive a call from TTSH, which is shifting beds across the road to the NCID — so could we be there in an hour?
As it turns out, the day before was, in Manauis’ words, “the most terrible Monday”. There was an attendance of 523 at the screening centre, which until today is the most people the centre has seen.
WATCH: An exclusive look inside the NCID screening centre (Dur 5:20)
“The patients (had to) wait outside (for) two hours. Inside, we really needed to run,” says senior staff nurse Yu Yong, who volunteered to triage patients at the screening centre the first chance she got.
Singapore’s border restrictions for several European countries had kicked in, and many of the students and workers who flew home translated into more suspect cases.
READ: PM Lee urges returning travellers to stay home, isolate themselves
The proverbial storm had arrived, just weeks after the country saw a slowing rate of infection. It was time to make room for potential admissions at the NCID, which shared resources with TTSH.
We make it to TTSH’s geriatric ward 9D in time. It is eerily quiet, if not for the 20-odd nurses gathered around the 20 beds meant to “double stack” wards at the NCID.

Confirmed COVID-19 patients were going to be put in isolation rooms of two, rather than have a room to themselves, as there was “no theoretical transmission risk”, says NCID clinical director Shawn Vasoo.
The NCID wards were designed to scale up from 330 to 586 beds, he adds.
After the nurses set off with the requisite equipment — down lifts, around bends, through doors, across a linkway connecting the two buildings — less than an hour and multiple trips later, NCID Ward 5F is stocked.
Even with beds already on standby at the NCID, opening a ward is not as simple as it sounds, or looks.
TTSH chief nurse Hoi Shu Yin recalls that Feb 5, a day after Singapore’s first community transmission happened, was one of the most stressful times for her department.
The patients who contracted the coronavirus while working at the Yong Thai Hang health products shop triggered a change in the definition of a suspect case, to include those in close contact with Chinese travellers.
The attendance at the screening centre jumped from about 70 to more than 300 overnight. Back then, anyone being checked at the screening centre was admitted for isolation as a precaution, and only four wards were open at NCID.
It took 100 beds, in less than 24 hours, and a lot of manpower to outpace the surge.
WATCH: CNA Insider exclusive: Inside TTSH's fight against COVID-19 (Dur 32:33)
READ: Inside Singapore’s COVID-19 screening centre, on the front line against the disease
“There’s a lot of coordination to make sure the medication’s there, the linens are there, the kitchens catered the bento food for our staff ... (since) they wouldn’t be able to leave the ward to purchase food,” Hoi says.
The materials management department supported them with supplies, the housekeeping team put up curtains and bedsheets in the wards, and engineers had to make sure the airflows were correct, says her counterpart, NCID nursing director Margaret Soon.
Since the day NCID opened in 2018, she adds, they have been drilled for this, but “it was a real test”.
On top of that, they have a military-inspired computer system to thank. Like the hospital’s nerve centre, the Command, Control and Communications (C3) system gathers data from all across TTSH-NCID, such as on supplies, patient flow and bed occupancy.

On the night the definition of a suspect case changed, C3 detected a surge of patients coming to the screening centre. The sustained high number “set off an alarm bell”, says TTSH chief operating officer Jamie Mervyn Lim.
“Very quickly, we activated the drawer plans,” he says. “We don’t want to be reactive, but (rather) to be ahead of the signs and signals that are presenting on the ground.”
By the time patients were admitted, there were enough beds for them.
THE PIVOT FROM FRONT LINE TO LAST LINE
On the same day the NCID’s capacity was expanded via the bed movement exercise, the Ministry of Health announced its first community isolation facility, D’Resort NTUC.
This was a “turning point” in Singapore’s isolation strategies, says Vasoo, whose job is to inform policymakers about clinical data from the ground.

With most of the cases sent to NCID before then, its clinicians learnt that age and medical history largely affected the severity of the virus infection.
“Most of the patients, thankfully, didn’t need ICU care. They didn’t need oxygen support. Their symptoms were mild, and generally they recovered uneventfully,” said Vasoo.
“We knew that such well patients probably shouldn’t be in an acute hospital bed … Those (beds) should be reserved for patients who are (sicker).”
His team then “came up with safe criteria to inform policymakers” about who were suitable for external care, the kind of monitoring the patients needed and the “criteria to re-refer these patients back to acute hospitals”.
Then came the peak of the pandemic in Singapore, when positive cases went up anywhere from over 400 to 1,000-plus daily among foreign workers. The need to conserve healthcare capacity was no more apparent than then.
The NCID’s wards were filling up again, and the centre activated its expansion plans.
Six general wards in TTSH were converted into isolation wards to house migrant workers who tested positive and needed hospital care. Those who were recovering well were discharged to community isolation facilities, like the Singapore Expo and Changi Exhibition Centre.
But was this all part of TTSH-NCID’s drawer plans? Were they really, as touted, always one step ahead of the pandemic? They were “flexible”, NCID executive director Leo Yee Sin replies with a wry smile.
While the Severe Acute Respiratory Syndrome (Sars) outbreak in 2003 lay the base for most of TTSH-NCID’s outbreak response, she was careful to answer whether they were more prepared for COVID-19, given that “outbreaks come in different shapes and sizes”.
“I’d say, we thought we were prepared because we had the past experience,” said the professor, who was part of Singapore’s Sars fight as an infectious diseases doctor.
A lot of times I think we kind of underestimated the Sars-CoV-2, or COVID-19.
But chief of what they learnt from past experiences with infectious diseases, she stressed, was flexibility.
“It may not already be in your plan, but you must have a system where it’s flexible enough so that it becomes situation-based and we can still respond effectively.”
To this end, being able to preserve healthcare capacity for those who require it, by moving patients into community isolation facilities, “enabled (the hospital) to save as many lives as possible”, says TTSH chief executive Eugene Fidelis Soh.
This was especially important during the peak of the pandemic here, he adds. And as far as war metaphors go for COVID-19, no one puts it quite like him.
“We started as the front line of the outbreak response,” he says. “As local transmissions started to occur in the community, the front line of the outbreak response shifted into the community.
“That meant we became the last line of defence.”
WHEN THE FIRST DEATHS STRUCK
While most of Singapore’s COVID-19 cases came and went without serious complications, a fraction wound up in the intensive care unit. On Mar 21, Singapore saw its first two deaths.
For ICU nurse clinician Gu Chunguang, this year’s experience in a pandemic has been sorely different from her nearly 20 years seeing “life and death almost every day”.

This time, “even in (the patient’s) last moment”, family members were not allowed to hold the patient’s hand and say their goodbyes properly.
“They need to say their goodbye (on) the phone,” says Gu. “What you all see is outside the ICU ward. What we see is the reality and the sickest patients among all the COVID-19 (cases) we have.
Unfortunately, some patients, because of their age or their co-morbidity … despite our every effort, still pass on.
When the physicians think the patient might die soon, Gu helps to coordinate with medical social workers on a time for family members to call the ward’s dedicated mobile phone.
Then, in personal protective equipment (PPE) and the phone in a Ziploc bag, she takes them to their loved one.
Some family members “respond (in) anger”, and in one case, fainted during the video call, Gu recalls. “We feel sorry for the family … we just feel helpless.”
And among the patients, she can “see fear in their eyes”.
“Imagine when you try to snorkel, you breathe through a straw. And when this straw is almost closed, and you’re gasping for air, you try to hold on to something, but you can’t hold on,” she says.
In those quiet moments, she would hold the patient’s hand. “Mr So-and-so, we’re here with you,” she would say. “We’ll do our best to make sure your last moment is comfortable.”
The ICU team — comprising physicians, respiratory therapists, pharmacists, among almost 16 roles — started seeing patients in February and were busiest in March and April.
They tended to young and old, locals and migrant workers. Most of the time, the patients were intubated for life support.

“The trajectory for critically ill patients … can be very tumultuous,” said Vera Lim, a consultant doctor in the department of anaesthesiology, intensive care and pain medicine.
A patient can become “very, very ill, very, very suddenly”, multiple organs could be deteriorating at once and the patient would need a concoction of about 10 types of medication.
That is where ICU pharmacist Neo Rui Yi comes in. “ICU patients really change (condition) hour to hour. So we do quite a lot of frequent dose adjustments,” she says.
A patient, at any point, has at least 12 to 13 healthcare professionals to provide round-the-clock care, say Ng Ziqin, a senior resident doctor in respiratory and critical care medicine.

Some of the sickest patients were migrant workers who were young and fit. Tending to these patients “was an emotional period for (her) personally”.
One worker who “etched a deep memory” was so ill he needed to be laid prone on his belly, “to improve the oxygen delivery to the lungs,” she recounts.
This takes five to six healthcare workers to do and is especially difficult if the patient is unconscious and hooked up to many tubes.
One of the toughest parts of the job, however, comes a step before helping the patient, says senior respiratory therapist Emelin Tan.
It comes when rushing to wear, in sequence, an N95 mask, goggles, shower cap, yellow gown and gloves, going through one door to an “anti-room” and then waiting for that door to close before the door to the patient opens — while the patient is gasping for air.
While necessary, it is the sense of helplessness that upsets Tan. “I have to get through all these physical barriers first, just to go in and offer reassurance,” she says.
Ultimately, she and the team try to remember that they are doing their best. “If a patient passes on … it’s more (about) how they passed on. That’s important to me,” she adds.
FAIL-SAFE, NOT FOOLPROOF: STAFF INFECTIONS
When it is all hands on deck to manage a pandemic, the last thing a hospital needs is an in-house cluster.
On Mar 30, in the thick of the imported cases, an NCID porter tested positive for COVID-19, the first of 10 staff infections (as of Aug 28).
In 2003, there were 97 probable Sars cases among healthcare workers, when TTSH was the main hospital dealing with the outbreak.
READ: 66 COVID-19 cases among healthcare workers and support staff
The porter was a 20-year-old Malaysian, who was in Malaysia from Mar 16 to 17 just before the country’s movement control order set in. He reported onset of symptoms on Mar 28 and was confirmed positive the next day.
The department of clinical epidemiology got down to work immediately.
It took one click on the staff surveillance system to identify his “first generation” contacts in the hospital, specifying those who had interacted with him for more than 30 minutes — thanks to a tracking device for everyone in the NCID.

“That helps us determine who’s a close contact versus someone who just walked past,” says Angela Chow, the doctor who leads the department.
If a contact was “unfortunately” not in PPE, “then we can quickly identify who had been exposed before the person becomes symptomatic”.
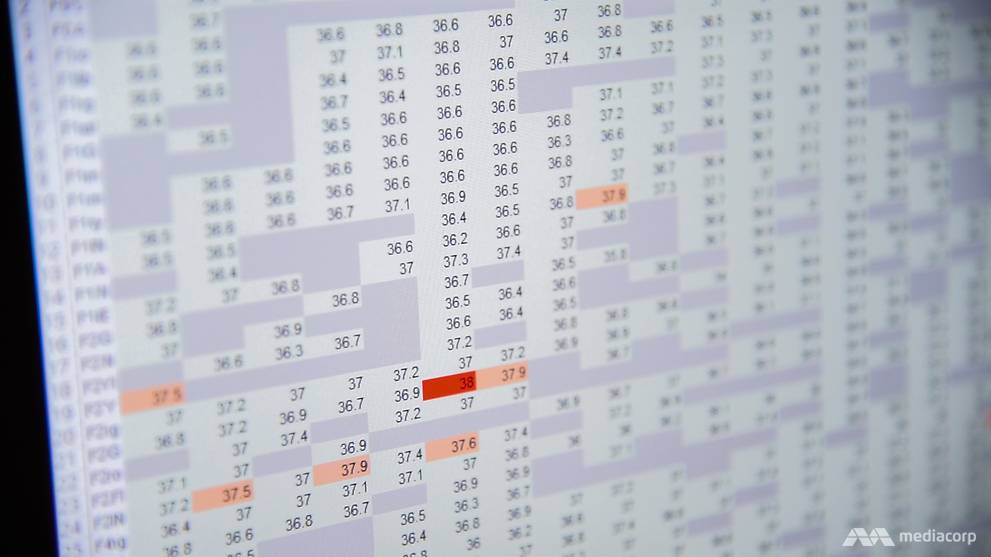
On top of the tracking system, all staff must input their temperature twice a day. A dedicated team watches this data closely, especially from those working at the screening centre and outbreak wards.
When staff fall sick with respiratory symptoms, TTSH-NCID “insists” that they visit the screening centre rather than a family doctor, to “close the gap as to where they’d go”, says Brenda Ang, the clinical director of TTSH’s infection prevention and control department.
“You could say this is Big Brother watching you, but just say this is a friendly father, a hospital observing people for staff safety."
Underlying the surveillance system are the hospital’s infection control measures, which hinge on basic things, like posters and instructional videos to remind staff how to don and doff their PPE safely. Every staff member, even contractors, is also “mask-fitted” for the most suitable N95 mask.
It was found that none of the 10 infected staff members contracted COVID-19 in the course of their work, notes Chow.
THAT MISLABELLING INCIDENT
More than half a year after work for COVID-19 began, with the microbiology laboratory’s testing capacity ramped up from 500 to 2,000 tests a day, Adjunct Assistant Professor Partha Pratim De’s nightmare comes true.
A mislabelling incident leads a student to be incorrectly diagnosed with COVID-19.

The TTSH head of laboratory medicine pushes back our interview, scheduled the next day, by a week. When we meet again, he tells us it was just not a good time.
“The honest answer is that it was a very simple, basic error. But around that, there were a whole lot of other contributory factors. A lot,” he says.
READ: Jurong West Secondary student incorrectly diagnosed with COVID-19, TTSH apologises for 'human error'
The Jurong West Secondary student had her specimen “cross-labelled” with a migrant worker’s owing to a “human error in the laboratory”, according to a TTSH media release on July 14.
With the case reclassified, the Education Ministry said there was no student-to-student transmission.
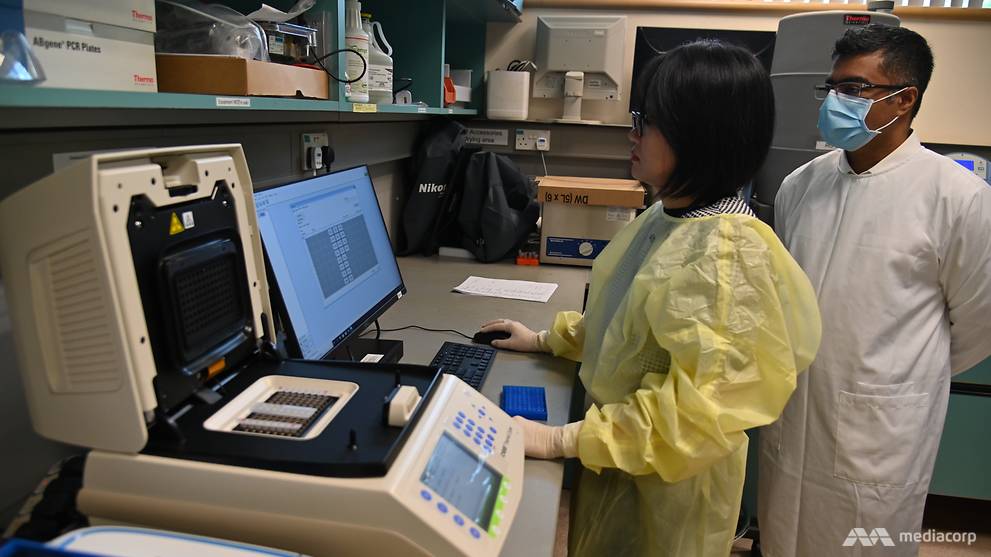
The polymerase chain reaction (PCR) test, as CNA Insider witnessed in our very first shoot inside the testing lab, is a very manual task.
WATCH: How COVID-19 testing is done in Singapore (7:10)
Lab technicians must be precise in handling, measuring and transferring the specimens, even in the wee hours, since COVID-19 testing was taking place 24/7.
“In the past, we were having to manually enter the patients’ details. And for a thousand of those, in the middle of the night, that’s quite a lot, when the PCR team is trying to do the more complicated, actual PCR work,” says Partha De.
“This was … distracting them, and they were more likely to make errors.”
READ: 'We can’t afford to make any mistake’: Inside a COVID-19 testing lab in Singapore
The patient registration and results entry processes are now automatic, “which helped to reduce the fatigue”. What machines cannot do, however, is relieve the “psychological demands” of the job.
“Even when we tell them to take their time … (the staff) have a very service-oriented mentality. They know there are patients waiting at the end of this, and they want to do their best,” says Partha De. “So we’ve had to try and manage all of that.
“I have to support them. I have to keep them going.”

READY FOR A SECOND WAVE
Asked how the past six months have been for him, he says one word “sums it up”. “Very tiring,” he replies with emphasis. “But it’s been necessary.”
While other hospital departments are gradually returning to pre-COVID-19, the lab’s workload has doubled as Singapore’s testing strategy expands. The lab almost hit its maximum capacity of 2,000 tests in 24 hours in July, and is averaging 1,000 a day.
“Previously we were doing diagnostic testing, which is of people who have symptoms,” says Partha De. “That’s now moved on to screening, which is testing of people who are well, who have no symptoms.”
They include construction workers, schoolteachers and delivery riders, to name a few.
The lab is “expecting that COVID-19 will become a new normal respiratory virus that we’ll test for every year”, as with swine flu, H1N1 and the seasonal flu. “Hopefully with a vaccine against it as well,” Partha De adds.
Places like Australia, Hong Kong, Japan and South Korea have seen a resurgence of COVID-19 cases. Despite the slowdown in Singapore, TTSH’s emergency department — while it has released its augmented manpower to their conventional roles — is not letting up.
“Every day, I’d look at the newspaper, and I’d see a little bit of an increase … in the community cases, and then we’d get worried,” said Manauis. The department is, however, prepared.
“In case of surges, we already have workflows in place … We have standby manpower that can be activated within eight hours,” she cites. “Our infrastructure’s already in place, so we’re ready.”
To ensure that doctors are not “de-skilled” regarding screening centre protocols, she continues to lead monthly trainings for doctors from the surgery, radiology, psychiatry and neurosurgery divisions, she says.

She is also training new staff continuously “so that existing medical staff don’t get burnt out”.
In a Talking Point episode, Lim the COO outlined some of the “contingency plans in place” for a second wave, such as standby beds and facilities, fully equipped.
“In 24 to 48 hours, we’re able to ramp up,” he told the programme.
As for other patient services, chairman of TTSH’s medical board, Associate Professor Chin Jing Jih, said a “hospital services prioritisation committee” has been formed.
“We get the doctors to prioritise many of the needs of these patients … That helps us to not overwhelm ourselves, and reserve some of this capacity in case a second wave arrives," he said.
“The principle is to ensure that patients are triaged according to their needs and those who require timely treatment aren’t deprived.”
TTSH-NCID have also collaborated with other hospitals to take on urgent cases “in the event (the hospital) is overwhelmed by demands”.
WATCH: COVID-19 second wave: Is Singapore ready? (21:08)
A SENSE OF DUTY
For all their plans, to Soh the CEO, the most important factor in the hospital’s state of readiness is its people.
“Our people choose to join TTSH, knowing that one day they may be called upon to serve in the front lines of an outbreak response here in Singapore,” he says.
“To them, this is a sense of duty.”
Dietetic technicians have rolled up their sleeves to help the security department marshal vehicles. Corporate communications specialists have taken on visitor registrations. And of course, doctors, nurses, allied health workers and ancillary staff have stepped up at the screening centre and outbreak wards.

It has been a united front against the pandemic. As of Sep 7, the NCID has admitted more than 4,000 patients with COVID-19 infection.
“I’m tremendously proud of my colleagues. They’re marvellous. They’re kind hearted, and they give the best in their care,” says Soh.
As for planning ahead, it is post-Sars 2003 all over again. “We learn with every outbreak. So for me, NCID will always be a work in progress.”